Aetna reveals health care denial rates in Medicare Advantage court case for NYC retirees
June 13, 2023, 4:58 p.m.
The company submitted a petition on Tuesday to intervene in a lawsuit that New York City retirees filed against the city and Mayor Eric Adams in Manhattan Supreme Court last month.
Aetna, the insurance provider chosen to service a health care switch for 250,000 municipal retirees, now wants a chance to defend the plan in court.
The company submitted a petition Tuesday to intervene in a lawsuit that New York City retirees filed against the city and Mayor Eric Adams in Manhattan Supreme Court last month. The lawsuit is the second attempt by city government retirees to block the Adams administration’s effort to switch them from traditional Medicare to a privatized version of the health care plan called Medicare Advantage.
In materials submitted to the court, Aetna outlines what it views as the merits of the new health plan and efforts to educate retirees about the changes underway.
Documents shared with Gothamist also showed that as of June 6, only 979 municipal retirees and dependents had opted out of the new Medicare Advantage plan. Members who opt out can either enroll in another alternative city plan, known as HIP VIP — or decline city coverage altogether and enroll in traditional Medicare independently. But they will lose city-funded benefits and have to pay for any supplemental coverage themselves.
The low number of opt-outs indicates that, “despite the noise about Medicare Advantage plans, retirees overwhelmingly like what they see in our plan,” according to Rick Frommeyer, senior vice president of Aetna’s Group Retiree Solutions.
But Marianne Pizzitola, a retired FDNY worker who serves as president of the NYC Organization of Public Service Retirees, said that’s because they weren’t given any good alternatives.
“The only people that would be willing to waive their city health benefits and all their reimbursements are high earners,” Pizzitola said.
Aetna’s move is the latest campaign to convince skeptical retirees and other vocal opponents of the merits of the shift.
According to Aetna, out of more than 82 million claims under its Medicare Advantage plans last year, only 3.4% were subject to prior approval, and 0.49% were denied.
New York City Comptroller Brad Lander declined to register the city’s contract with Aetna last week, citing the ongoing lawsuit.
“I am seriously concerned about the privatization of Medicare plans, overbilling by insurance companies, and barriers to care under Medicare Advantage,” Lander said in a statement at the time.
Lander stated that the decision was based purely on procedural concerns, but his office told Gothamist this week that the mayor could override the move.
Nine retired city workers filed the lawsuit — along with the NYC Organization of Public Service Retirees, a group that formed to fight the Medicare Advantage shift. They claim that the Adams administration is violating city law by diminishing their benefits and not paying for SeniorCare, the supplemental coverage that was previously provided by the city at no cost to city workers.
Aetna, Adams and a committee of municipal labor unions collaborated on the plan and have argued that the new benefits will be comparable – if not better – than what members previously had, without increasing their out-of-pocket costs. Plus, the plan is designed to save the city an estimated $600 million a year on health benefits, thanks to federal funding available for Medicare Advantage plans.
Adams previously sought to maintain the option for retirees to stay on traditional Medicare, with the Senior Care supplement, for a fee of $191 a month. But that move was blocked in court because it would violate the city’s administrative code. As a result, Adams eliminated that option altogether.
Now, if the switch goes forward, some 250,000 municipal retirees and their dependents will be shifted to Aetna’s Medicare Advantage plan automatically on Sept. 1. June 30 is the deadline for opting out, and another window will not arrive until next year’s enrollment period.
Will city retirees be denied care?
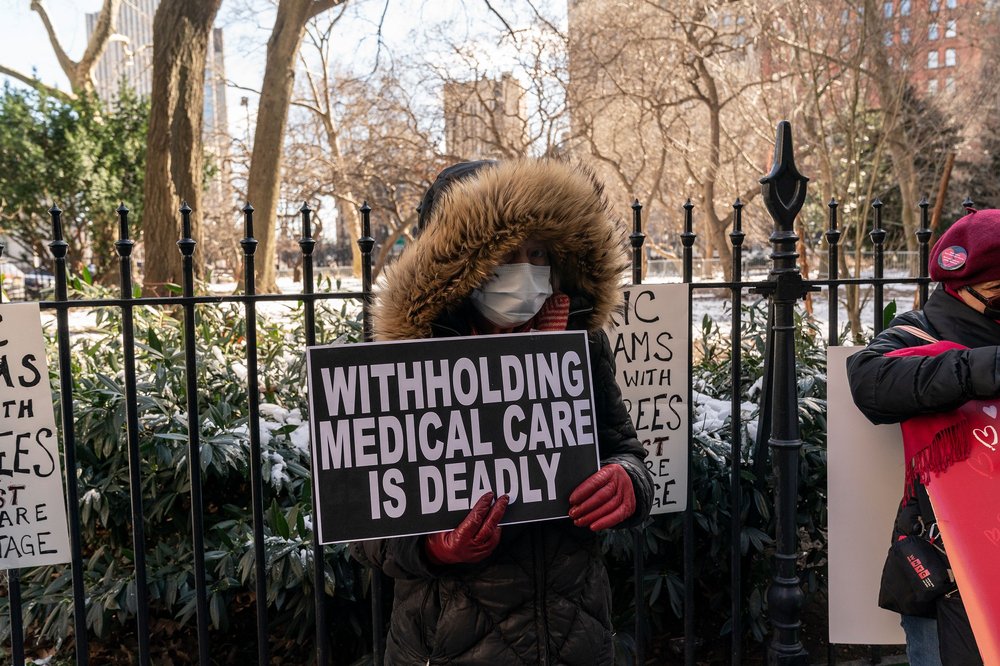
Pizzitola and others who oppose the switch have raised concerns about the need for doctors to get prior approval for more services under Medicare Advantage than traditional Medicare – and a federal investigation has revealed that under Medicare Advantage plans, claims are sometimes inappropriately denied.
Aetna is seeking to demonstrate — via materials submitted to the court — that its existing Medicare Advantage plans across the country rarely reject coverage for needed health services. Those documents outline how those denials would be even more infrequent under its plan for New York City government retirees.
According to Aetna, out of more than 82 million claims under its Medicare Advantage plans last year, only 3.4% were subject to prior approval, and 0.49% of all claims were denied. That still amounts to at least 401,000 claims denied. Based on those figures, Aetna rejected about 14.4% of the claims that were submitted for prior approval.
In 2021, the company’s Medicare Advantage plans either partially or fully denied about 12% of requests for prior approval, tied for the highest denial rate of major insurance companies studied by the health policy nonprofit KFF. Aetna has said that the denial rate would be lower for New York City’s plan.
“I have no basis to challenge their numbers,” said Barbara Caress, who teaches health policy at Baruch College and previously served as director of strategic and policy planning for the union 32BJ’s benefit funds.
But she said the numbers don’t capture the phenomenon of doctors not bothering to seek prior approval for medical services they assume will be rejected under Medicare Advantage. Caress said she would be curious whether Aetna ultimately denies services that are more expensive – as opposed to procedures that are truly not recommended or deemed unnecessary.
Caress said it will be necessary to review how people use their health benefits in the first year of the Medicare Advantage plan if it goes through.
Have you had coverage under a Medicare Advantage plan in New York City? We want to hear about your experience. Email Caroline Lewis at clewis@wnyc.org.
This story was updated with additional information on Aetna’s denial rates.
It's official: NYC inks deal with Aetna on new Medicare Advantage plan for 250K retirees 250K NYC retirees must switch to new Medicare coverage after union leaders favor privatized plan